MAURITANIA

By 2050, the population of Mauritania is expected to increase by half, reaching 6 million inhabitants, which will lead to significant repercussions on the country’s socio-economic development in the fields of health, education, housing, employment and food. At present, 31% of the population lives below the poverty line, with significant disparities between those living in rural areas (44.4%) and in urban settings (16.7%)*. The overall mortality rate across the population as a whole remains high (8.5‰), despite major investment in sexual and reproductive health, neonatal and adolescent health in recent years. Although malaria is one of the main drivers of mortality, other afflictions such as tuberculosis, hepatitis B, malnutrition or recurrent epidemics such as viral haemorrhagic fevers, cholera and Ebola virus disease are all major public health problems. Ensuring access to healthcare services for all is fraught with geographic and financial barriers. Healthcare infrastructure, especially in rural areas struggles to provide quality services and optimal management of medicines and vaccines.
*Source: FORSS Programme – SIRA Haby Ba, Status report on services available in the struggle against HIV/AIDS in Mauritania, April 2019 (in French)
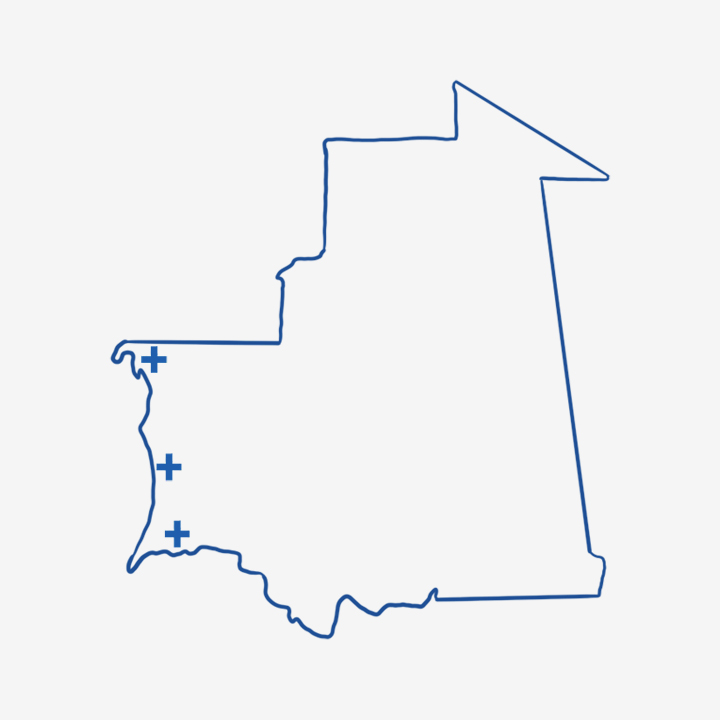
Very limited geographical coverage for HIV-related services
Although a positive shift in the figures relating to HIV testing has been observed since 2002 thanks to the creation of dedicated centres, the involvement of civil society in mobile testing and the adoption of a national strategy in 2020, the sector continues to suffer from numerous shortcomings. Just 58% of the territory is covered and few of the centres are actually functional or communicate sufficiently about their activities to the extent that free screening can only really be accessed in a handful of places*. In addition, the country has just seven treatment centres (in Nouakchott, Nouadhibou, Kiffa, Kaédi, Néma, Zouérate and Rosso) Hundreds of people therefore have to travel up to 800km in order to reach their nearest treatment centre, exacerbating the issue of patients dropping out of treatment and making access to other components of comprehensive support (such as nutritional and psychosocial monitoring and educational therapy) much more difficult. Just 8% of medical staff have been trained in dealing with PLHIV. Furthermore, the treatment units themselves are characterised by their very small buildings that host several activities. This in turn raises issues about the lack of confidentiality and explains why some of the PLHIV prefer to keep their distance from the services offered at such sites.
*Source: FORSS Programme – SIRA Haby Ba, Status report on services available in the struggle against HIV/AIDS in Mauritania, April 2019
KEY FIGURES
UNAIDS 2023 – MAURITANIA
of PLHIV who are aware of their HIV status receive antiretroviral treatment
HIV prevalence rate among sex workers.
HIV prevalence rate among men who have sex with men (MSM).

Groups that are especially “at risk”
The low prevalence of the HIV/AIDS epidemic in the country (0.3% in 2021) masks significant disparities. The epidemic has a focal points in urban areas (reaching 1.66% in Nouadhibou, for example) and within groups said to be “at risk”, notably among men who have sex with men (MSM) (23.4%)* and among sex workers (SW) (9%)**. The vulnerability of these groups increases with a high prevalence rate of sexually transmitted infections and limited knowledge regarding modes of transmission. Some of the determinants often cited include poverty, migration and multiple marriages. However, those said to be “at risk” and key populations also and above all face a discriminatory legislative, cultural and social environment.
*Source: UNAIDS 2021 statistics
**Source: Ibid.
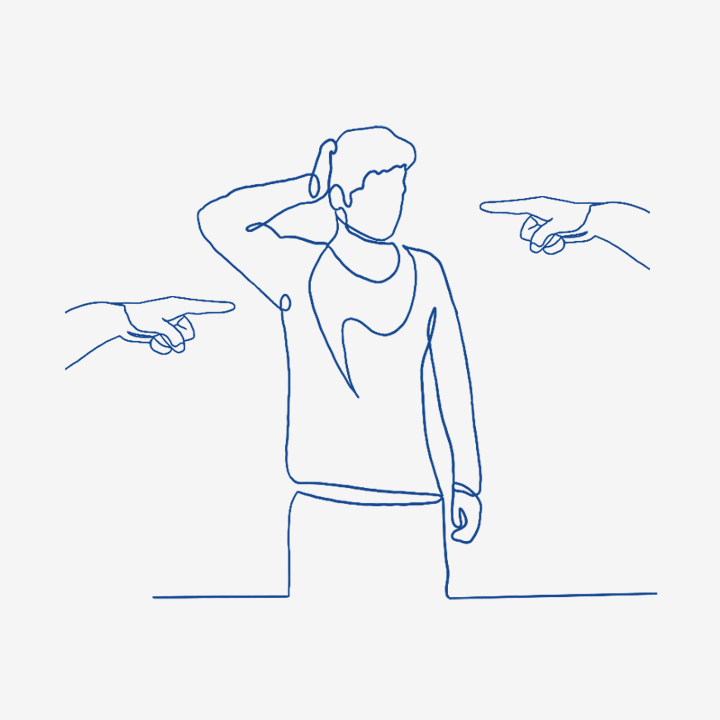
Key populations are heavily stigmatised
Mauritania is one of a number of countries where sexual relations between members of the same sex is subject to the death penalty (Art.308 of the Penal Code). Although the law is not applied in practice, MSM are regularly imprisoned or victims of harassment by law enforcement officers. Among them, PLHIV say they suffer discrimination from nursing staff and highlight rejection and a lack of confidentiality. Alongside widespread mistrust of MSM and PLHIV among the Mauritanian population, this criminalisation and stigmatisation explains many of the healthcare failings. As regards sex work – officially banned – it is driven underground. SW report difficulties in getting access to information and means of prevention, but also in accessing protection for their rights, particularly in cases where they are stopped by the departments tasked with “combating moral depravity”. Possession of condoms, for instance, warrants arrest by the police. Given the high level of stigmatisation that SW reportedly experience from nursing staff, especially in public health facilities, the relief provided by civil society organisations seems all the more critical.